My cancer might be back—and I wonder if unnecessary radiation caused it in the first place
Fortune,

I was a 23-year-old investment banker, working ludicrous hours in New York and training for marathons on the side, when cancer first entered my life. In the three decades since, the disease has been perhaps not a constant companion, but certainly a ride-along. I did not always hear it; it was not always speaking loudly. But it was back there somewhere.
And now that there is a possibility that my cancer has returned, questions about some of the decisions my doctors and I made in those early days have resurfaced.
Was my radiation really necessary? Could we have more thoroughly discussed the poor base of research related to my type of cancer, and would knowing more about the uncertainties and potential long-term complications have made a difference in my choices?
Is the way we treated my cancer back then the reason I’m still here 30 years later, or is it the cause of the new nodules discovered in my neck? Both?
On a daily basis in the U.S., unnecessary medical tests, treatments, and surgeries actively harm patients at astounding rates. Physicians fail to adequately inform subjects about the downstream risk of procedures. The pharmaceutical and biomedical industries influence doctors’ decision-making, actively bias major product research, pay key players to grease the skids for expanded sales, and ignore or obscure the harm some of their medicines and devices can do.
Patients, many of them vulnerable and afraid, are suggestible in the extreme—and the COVID-19 pandemic has only underscored that truth. By the time they realize that one ill-fated decision may lead to more and more medical intervention and costs, it’s often too late.
This is by no means a full picture of the health care industry, but it may be the piece that is the least well understood. In my case, I likely would have come to many of these conclusions on my own—hard-won knowledge from 30 years spent living with a disease.
But I will never have to test that theory, because I have already seen it all firsthand. From the other side of the gurney.
Not long after I began my work as an emergency department physician, a few years after my own diagnosis, the ER director singled me out as the department’s “top income generator on a per-hour basis,” a designation that I was not aware existed. He said he wanted to know my secret.
My secret: I was inexperienced and afraid of missing something, so I was ordering too many tests and likely hospitalizing too many patients. But my boss wasn’t complaining.
As a health care consumer in America, you are far more likely to be steered toward needless tests and procedures than away from them. Such unnecessary testing and surgeries add up to more than $200 billion in extra spending per year, according to the Institute of Medicine. At least 30,000 deaths in the U.S. each year are linked to mistakes and injuries caused by superfluous medical procedures. In a 2017 survey, doctors from the American Medical Association said that nearly a quarter of all the tests they performed were unnecessary, along with more than 20% of the prescriptions they wrote and every 10th surgery.
I neither knew nor thought about any of this when I was diagnosed at the age of 23; I wanted help. The tumor on the roof of my mouth had grown, gradually but persistently, until it was the size of a golf ball. After initial care back home in Texas, doctors at Memorial Sloan Kettering Cancer Center ran more tests that confirmed their suspicion: I had a rare form of salivary gland cancer, and the tumor itself was sitting atop a large artery. It was delicate and dangerous, and it would take two surgeries to get it all.
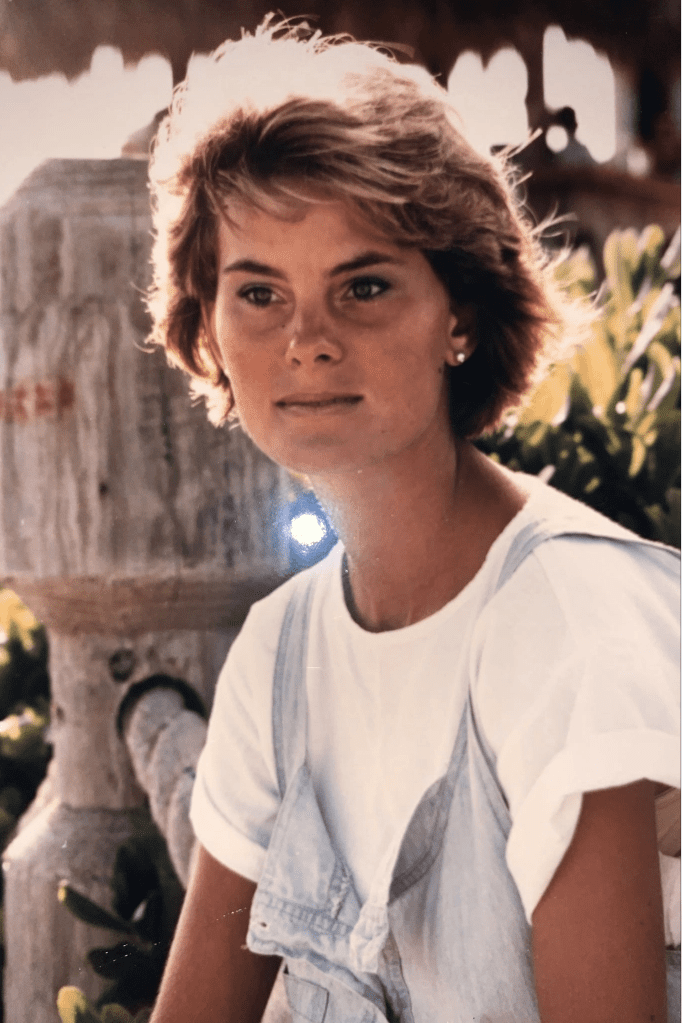
Dr. Carolyn Barber in 1987.
What followed led me to my current life path. Inspired by the care and support I received, I left banking, eventually entered the Johns Hopkins University School of Medicine, and completed a residency at Stanford University Medical Center. I have spent the past 25 years caring for patients in the emergency departments of several teaching hospitals, an absolute privilege and a meaningful way for me to give back.
But there was another component to my case back then: With little discussion beforehand, I underwent radiation therapy as a complementary treatment to my surgeries. My radiation oncologist briefed me on a few of the potential short-term effects of such treatments. The long-term risks? Not so much.
Some of the complications from those treatments have changed my daily life forever. Significantly, a procedure to close a small hole on the roof of my mouth by using a skin flap failed immediately, very likely because of the prior radiation. The hole became much larger, and it now affects my speech to the point that I am often misunderstood, especially on the phone. I experience chronic sinusitis and headaches with fairly frequent acute infections.
Radiation may have been the right call at the time; we didn’t have a lot to go on, as my diagnosis was unusual. But the complications were severe, and some were not discussed. We are more aware now of the risks associated with many treatments—and, for some, the stunningly low rates of effectiveness. But such treatments continue to be pushed, and they make money—for medical companies, device makers, drug manufacturers, and, sometimes, doctors.
If you’re an average adult, you likely know someone who has had a cardiac stent implanted to fight coronary disease. In the U.S., we place such stents in an estimated 100,000 patients each year who have stable heart disease, at a cost of roughly $30,000 per procedure, though prices vary considerably. High-quality scientific studies show that stents in stable patients neither save more lives nor reduce the odds of a heart attack any more effectively than simply taking heart medicine and making lifestyle changes. But they are profitable.
Spinal fusion? It’s a $40 billion annual industry, the most popular elective surgery in the U.S.It also seldom works: Multiple studies show it to be no more effective than nonoperative treatment (such as physical therapy) in patients with chronic low back pain. And, discectomies, wildly popular procedures for those with herniated discs, have repeatedly been proved no more effective over the long term than having no surgery at all. Perhaps more concerning, the rate of complications from these back surgeries runs as high as 18% to 20%.
Overaggressive, unnecessary treatment can lead to patient harm, reoperations, longer stays, more studies, more tests, and more imaging, all at a high cost to the patient. Meanwhile, the money rolls in for three significant players: hospitals, Big Pharma, and medical device manufacturers.
Often, when patients find themselves steered toward a particular line of treatment—a certain medication, say, or a procedure calling for a specific brand of device—their doctors make these recommendations based on studies that appear to support the plan. In truth, these studies may well have been bought and paid for by the product’s manufacturer.
Our medical literature is often fraught with bias in favor of certain products, because the drug and medical device companies sponsor so much of the research. Their methods often lack rigor. A large study by the preeminent research review organization Cochrane concluded that industry-sponsored research was three times as likely as nonprofit-funded work to recommend the sponsor’s own drug.
Biased data can become scientific fact. It can also take a long time to undo. A 10-year survey of research articles published in The New England Journal of Medicine (NEJM) showed that 40% of established medical practices were later found to be invalid. By the time the medical community realizes a drug doesn’t work, Big Pharma has made its money and moved on to promoting the next one.
Do you take a statin, like Lipitor or Crestor, despite being an otherwise healthy person? The statin industry is remarkably lucrative in the U.S. on the premise that statins can help prevent a first heart attack, in addition to their uses for those who already have coronary heart disease. But tests of their effectiveness and need have come to wildly differing conclusions.
A meta-analysis involving 65,000 patients concluded that statins do not offer a mortality benefit to people without heart disease who use it as preventative medicine. The drugs have been credibly linked to an increased risk of diabetes, memory loss, and muscle weakness. Yet they continue to be prescribed and taken by some 35 million Americans.
How does this happen? The pharmaceutical industry has two primary pathways: paying for and thus controlling the results of research, and mass marketing to physicians via gifts, free drug samples, grants, paid speaking engagements, and more.
They’re not subtle. One company, Medtronic, sponsored 13 different studies that supported the use of its drug, Infuse, to improve outcomes for various back surgeries. None of the 13 trials reported any complications. But an independent article reported “frequent and occasionally catastrophic complications” associated with the drug’s use in spinal fusion surgeries. Why the discrepancy? Well, Medtronic had paid the authors of its studies $210 million for “consulting, royalty, and other miscellaneous arrangements” over a 14-year period and steered the content written by its paid experts, according to the Senate Finance Committee.
Well-meaning physicians can make inappropriate decisions for their patients based on such manipulated research. The concept of evidence-based medicine, for so long a hallmark of trustworthiness, has been deeply corrupted by drug and device manufacturers whose deep pockets can sway the results and the reporting.
From the time a doctor is a medical student, industry marketers cater lunches, bring gifts, offer free gatherings at expensive restaurants under the guise of “medical training,” and fund national conferences. As physicians gain seniority, they may be hired for industry speaking engagements worth thousands of dollars, or paid six figures to sit on a company’s board. A physician may even be given stock options or receive patent royalties from an invention.
Spending money works. A ProPublica 2019 analysis of 50 popular medications across all specialties found that doctors who received payments from Big Pharma wrote 58% more prescriptions of a drug, on average, than physicians without these ties. Novartis recently settled for $678 million a fraud lawsuit in which it was accused of paying kickbacks to physicians to prescribe its drugs.
The National Comprehensive Cancer Network’s 2019 guidelines encourage cancer patients to participate in some of the 300,000 clinical trials being conducted globally. But their oncologists may be in conflict, since some of them are paid “finder’s fees” and bonus payments for patient recruitment, totaling tens of thousands of dollars, from the drug manufacturers themselves. A JAMA study, meanwhile, found that among 71 cancer drugs approved for solid tumors, median survival increased by only 2.1 more months than with existing medicines. Imagine the poor survival odds for many patients in untested clinical trials.
Recently, a screening ultrasound revealed two suspicious nodules in my neck, leading to worry that my cancer might have returned after 30 years. I consulted a respected outside oncologist, who suggested a complete neck dissection, potential new radiation, and a chest CT scan to look for metastases—yet he agreed that none of it would improve survival chances. My own doctors advocated for watchful waiting, which is where I’m headed.
This possible recurrence may have something to do with the radiation treatment I received in 1987; it may not. Regardless, I didn’t know any better at the time. Doesn’t that describe a majority of us in most critical medical situations?
That has to change. Our hospitals and medical specialty organizations can help reduce overtesting by uncoupling physician pay and test ordering. They can move away from the fee-for-service model and toward value-based care. They can seek medical tort reform to reduce the don’t-get-sued pressure physicians feel to advocate for more tests or procedures.
I second several of the recommendations made by Dr. Marcia Angell, a former editor-in-chief of the NEJM: Industry should not be allowed to sponsor its own clinical trials. Big Pharma should not be funding physicians’ medical educations or sponsoring national symposia. And direct-to-consumer sales pitches by industry should be eliminated to reduce patients’ demands for drugs and testing.
We also need a plan to finance medical education. Being $200,000 in debt can be a powerful inducement to say yes when Big Pharma and the medical device industry come calling.
Finally, as physicians, we need to do the lion’s share of the work. We need to read primarily non-industry-funded research and more openly discuss risks versus benefits of nonessential treatment. Sometimes, we need to be willing to draw upon our experience and recommend doing nothing. If collectively we can cut unnecessary services by half, the Institute of Medicine estimates health care expenditures will drop by $105 billion every year.
I’m extremely grateful for medicine, for my care, and for being alive. I have worked with and among many wonderful physicians, and I can attest that their jobs are difficult and challenging. Many pharmaceutical and medical device companies have made significant advances in health care. But we must do better.
And sometimes we do. My two personal oncology physicians were the ones who advised a conservative strategy of monitoring those nodules in my neck, which could prove to be benign. They believe the risk of surgically removing them, with all of the potential complications, far outweighs the benefit. I’m ever appreciative of their reflection, care, and honesty. I believe they deeply honor the aphorism: First, do no harm.
Carolyn Barber earned her BA from Princeton University, did her medical training at Johns Hopkins University School of Medicine, and completed her residency at Stanford University Medical Center. An emergency department physician for 25 years, she is also cofounder of a homeless work program, Wheels of Change, and a nationally published author. This article is adapted from her new book, Runaway Medicine: What You Don’t Know May Kill You, which was recently Amazon’s top-ranked bestseller in health care administration.
